Convalescent plasma therapy holds key for the immediate treatment of severely sick COVID-19 patients. This article discusses effectiveness of this therapy and its present status about its use in treating COVID-19
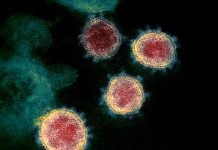
The COVID-19 disease has engulfed the entire world with varied effects in different countries with respect to infected individuals and mortality rates. Around 2 million people have contracted the disease globally and numbers are rising daily. Till date, there is no prescribed and approved treatment for this disease. The entire medical fraternity is eagerly waiting for a treatment that can not only provide cure for the infected people but also prevent the non-infected healthy individuals from this disease. Pharma and biotech companies and research institutes globally have already begun researching on several approaches to find a cure for COVID-19. These approaches include use of small molecule drugs (1), vaccine development (2) and antibody therapy (3). However, all these approaches will lead to a treatment regimen that would take at least a year or a couple of years before a treatment is approved by the regulatory authorities, even as a fast track approval for emergency use. The need of the hour is to find an immediate treatment that can bring relief to the victims of COVID-19. Convalescent plasma therapy (CPT) is one such treatment that can be used to treat infected patients in the short term while waiting for the other therapies to develop. This article will discuss about the history and concept of convalescent plasma therapy, its relevance and effectiveness in treating COVID-19 patients and the approach taken by medical and regulatory authorities globally for its use.
The history of CPT dates back to 1890s, when a German physiologist, Emil von Behring, was successful in treating animals infected with diptheria using serum from animals that were immunized with attenuated forms of diptheria causing corynebacterium. The antibodies present in the serum from immunized animals prevented infected animals from getting the disease.
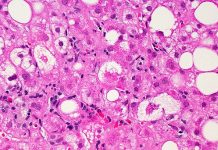
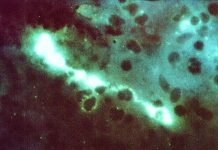
Convalescent plasma therapy involves isolating the plasma from infected individuals that have recovered from the disease and injecting it into the patients with disease, thereby providing passive immunity from the plasma containing antibodies generated against the pathogen in recovered individuals. The process consists of drawing blood from donors that have recovered from the disease, separating the plasma and checking the antibody titre before administering it to the infected patients. This therapy has been successfully used previously for the Spanish flu pandemic of 1918, Ebola, SARS, MERS, and 2009 H1N1 pandemic (4-9). In case of Spanish flu, the mortality rates were reduced to 50% for infected patients that were given CPT in comparison to those who didn’t (10), with the primitive technologies present at that time for separating plasma from blood. Due to the similarities of these disease causing viruses along with their clinical characteristics with the SARS-CoV-2 virus, convalescent plasma therapy may prove to be a good choice for treatment of infected patients with plasma from the donors that have recovered from the COVID-19 disease. In case of COVID-19, the number of recovered patients hold the key to the success of the plasma therapy. Interestingly and on the positive side, as of April 16th 2020, 25% of the infected patients with COVID-19 (equivalent to ~ 523,000 people globally) have recovered (11) and plasma from these individuals can be used as an immediate and short term treatment of infected people, especially those showing severe symptoms.
Countries across the world have either already started or in the process of approving CPT for investigational use for the treatment of COVID-19. A limited small trial in China for CPT on 10 patients (six males and four females) with a median age of 52.5 years was conducted with primary outcome of safety and secondary outcome of improvement of clinical symptoms. The therapy was well tolerated without any adverse effects and there was a significant reduction in clinical symptoms within 3 days of administering the therapy (12), although the effect and time taken for patients to be SARS-CoV-2 negative, varied in different patients. This has provided enough relevance and hope for the CPT to be further used in clinical trials in other regions of the world affected by COVID-19.
The apex body of medical research in India, ICMR (Indian Council of Medical Research) has given permission to Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST) in Kerala for carrying out CPT in a clinical trial setting (13). The study would be conducted on a small number of patients who are severely infected with COVID-19 in partnership with five medical college hospitals. Severely infected patients represent those that are in intensive care experiencing shortness of breath, low blood oxygen saturation levels (less than 93%), septic shock and/or multiple organ impairment including ones that are about to be put on a ventilator. ICMR has also solicited cooperation from other medical researchers across the country to engage in clinical trials using CPT for COVID-19 patients with an aim to assess the safety and efficacy of this procedure (14).
European Union has also endorsed the use of CPT as a promising treatment for COVID-19 and is seeking help from member States for collecting blood from recovered donors for carrying out CPT (15). It is also building a database in partnership with European Blood Alliance (EBA), for blood collection and the outcome of clinical trials, that will be shared with member States.
National Health Services (NHS) in UK is also soliciting patients who have recovered from COVID-19 to donate their blood through various centres across the UK in order to start clinical trials of CPT for the severely ill COVID-19 patients (16).
US FDA on April 13th 2020, issued guidance to use CPT as an investigational procedure in a clinical trial under the traditional IND regulatory pathway (21 CFR Part 312) for patients affected severely by COVID-19 (17). The responsibility of reviewing requests from sponsors would be undertaken by the office of Blood Research and Review, a unit of CBER (Center for Biologics Evaluation and Research).
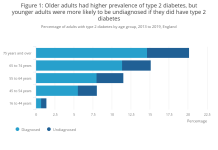
As with all other therapies, CPT also comes with its own challenges. The first and foremost is to get access to the recovered patients and convincing them to donate their plasma. The recovered individuals should be free of any other disease condition, which is a real issue in case of COVID-19 where majority of victims are aged people who might have a history of other medical complications such as heart disease, diabetes, blood pressure etc. Plasma obtained should be in sufficient quantities and have a high antibody titer so that enough people can benefit from the same. Blood from plasma donors would have to undergo testing for infectious agents and blood group compatibility with the recipient. All this would require a massive coordination between the medical personnel, agreed donors that have recovered from the disease and the patients receiving CPT, for the entire procedure to yield a successful outcome.
Nonetheless, notwithstanding the shortcomings, CPT still holds promise, with safety and efficacy being prime attributes, for the short-term treatment of COVID-19 patients. If CPT for Spanish flu can reduce the mortality rate to 50%, it is surmised that the reduction in mortality rate using CPT for COVID-19 should be greater than 80%, keeping in mind the present state-of-the-art technologies for plasma separation, storage and administration accompanied with modern patient care facilities. The medical fraternity should leave no stone unturned to exploit CPT for the treatment of COVID-19 patients until a small molecule, vaccine or antibody therapy is approved which would take its own course of time with the hope of vaccine being developed the fastest (one to two years), followed by novel small molecule(s) and/or repurposing of existing small molecular drugs and antibody therapy.
***
References:
1. Gordon CJ, Tchesnokov EP, et al 2020. Remdesivir is a direct-acting antiviral that inhibits RNA-dependent RNA polymerase from severe acute respiratory syndrome coronavirus 2 with high potency. J Biol Chem. 2020. First Published on April 13, 2020. DOI: http://doi.org/10.1074/jbc.RA120.013679
2. Soni R., 2020. Vaccines for COVID-19: Race Against Time. Scientific European. Published on 14 April 2020. Available online at http://scientificeuropean.co.uk/vaccines-for-covid-19-race-against-time Accessed on 16 April 2020.
3. Temple University 2020. Temple Treats First Patient in the U.S. in Clinical Trial of Gimsilumab for Patients with COVID-19 and Acute Respiratory Distress Syndrome. Lewis Katz School of Medicine News Room Posted on 15 April 2020. Available online at https://medicine.temple.edu/news/temple-treats-first-patient-us-clinical-trial-gimsilumab-patients-covid-19-and-acute Accessed on 16 April 2020.
4. Mupapa K, Massamba M, et al 1999. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. The Journal of Infectious Diseases, Volume 179, Issue Supplement_1, February 1999, Pages S18–S23. DOI: https://doi.org/10.1086/514298
5. Garraudab O, F.Heshmati F. et al 2016. Plasma therapy against infectious pathogens, as of yesterday, today and tomorrow. Transfus Clin Biol. 2016 Feb;23(1):39-44. DOI: https://doi.org/10.1016/j.tracli.2015.12.003
6. Cheng Y, Wong R, et al 2005. Use of convalescent plasma therapy in SARS patients in Hong Kong. Eur. J. Clin. Microbiol. Infect. Dis. 24, 44–46 (2005). DOI: http://doi.org/10.1007/s10096-004-1271-9
7. Zhou B, Zhong N, and Guan Y. 2007. Treatment with convalescent plasma for influenza A (H5N1) infection. N Engl J Med. 2007 Oct 4;357(14):1450-1. DOI: http://doi.org/10.1056/NEJMc070359
8. Hung IF, To KK, et al 2011. Convalescent plasma treatment reduced mortality in patients with severe pandemic influenza A (H1N1) 2009 virus infection. Clin Infect Dis. 2011 Feb 15;52(4):447-56. DOI: http://doi.org/10.1093/cid/ciq106
9. Ko JH, Seok H et al 2018. Challenges of convalescent plasma infusion therapy in Middle East respiratory coronavirus infection: A single centre experience. Antivir. Ther. 23, 617–622 (2018). DOI: http://doi.org/10.3851/IMP3243
10. Dave R 2020. Before Vaccines, Doctors ‘Borrowed’ Antibodies from Recovered Patients to Save Lives. Available online at https://www.history.com/news/blood-plasma-covid-19-measles-spanish-flu Accessed on 16 April 2020.
11. Worldometer 2020. COVID-19 CORONAVIRUS PANDEMIC. Last updated: April 16, 2020, 12:24 GMT. Available online at https://worldometers.info/coronavirus/https://worldometers.info/coronavirus/ Accessed on 16 April 2020.
12. Duan K, Liu B et al 2020. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. PNAS first published April 6, 2020. DOI: https://doi.org/10.1073/pnas.2004168117
13. PIB 2020. ICMR approves Sree Chitra Institute in Kerala to conduct clinical trials using convalescent plasma therapy for COVID-19 patients. 11 April 2020. Available online at https://pib.gov.in/newsite/PrintRelease.aspx?relid=201175. Accessed on 17 April 2020.
14. ICMR 2020. Call for Letter of Intent for Participation in: Therapeutic Plasma Exchange in COVID-19: Protocol for a Multi-center, Phase II, Open Label, Randomized Controlled Study. Available online at https://icmr.nic.in/sites/deult/files/upload_documents/LOI_TPE_12042020.pdf Accessed on 17 April 2020.
15. EU, 2020. Guidance on the collection and transfusion of convalescent COVID-19 plasma. Version 1.0 April 4 2020. Available online at https://ec.europa.eu/health/blood_tissues_organs/covid-19_en. Accessed on 17 April 2020.
16. NHS 2020. Could you donate plasma to help treat coronavirus (COVID-19) patients? Clinical trial. Available online at https://www.nhsbt.nhs.uk/how-you-can-help/convalescent-plasma-clinical-trial/ Accessed on 17 April 2020
17. FDA 2020. Recommendations for Investigational COVID-19 Convalescent Plasma. Posted 13 April 2020. Available online at https://www.fda.gov/vaccines-blood-biologics/investigational-new-drug-ind-or-device-exemption-ide-process-cber/recommendations-investigational-covid-19-convalescent-plasma Accessed on 17 April 2020.
***